Cervical Cancer
Cervical cancer can almost always be avoided with regular screening, getting the human papillomavirus (HPV) vaccine and following up on abnormal results.
What is cervical cancer?
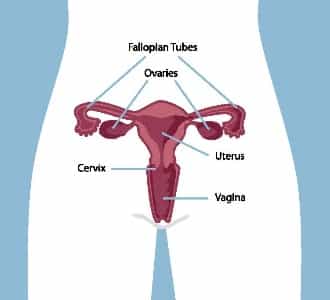
Cervical cancer can develop when cells in the cervix grow uncontrollably and are not treated. Most often, these uncontrolled cell changes are caused by the human papillomavirus (HPV).
What is the human papillomavirus (HPV)?
Human papillomavirus (HPV) is a common virus that affects most people at some point in their lifetime. Around 100 types of HPV can affect different parts of the body, but most are harmless and go away on their own. About 15 of these are considered “high-risk” and can cause abnormal cells to develop in the cervix that can lead to cervical cancer if left undetected.
Getting the HPV vaccine can help protect you against certain types of HPV. HPV spreads very easily — at least 7 out of 10 people will get it at some point in their lives. Almost all cases of cervical cancer are caused by HPV. But the types of HPV that can cause cervical cancer usually don’t cause symptoms, so most people don’t even know they have it. Oftentimes the body fights the infection and the virus goes away on its own within 2 years and without any serious issues.
Is there a cure for HPV?
Unfortunately, there’s no cure for HPV and it can’t be treated with antibiotics. Deciding to have a Pap test regularly is the best thing you can do to help make sure abnormal cervical cells caused by HPV are found early. When found early, these cells can be treated so that cervical cancer doesn’t develop.
HPV is easily spread by even brief skin-to-skin contact in the genital area. You don’t have to have sexual intercourse to get HPV – you can get it through oral sex or simply by touching. The high-risk types of HPV don’t cause symptoms, so most people don’t even know they have it – or that they’re passing it on to their partner. The virus can hide in your body for years without any symptoms.
Testing for HPV
If you’re 30 years or older, and the lab sees cell changes that are hard to read, your Pap test sample may be tested for HPV. This is called HPV reflex testing. If you’re under 30, your Pap test sample won’t be tested for HPV, as it will normally clear up on its own.
Risk factors (things that can increase your risk)
HPV is very common in anyone who is sexually active. That’s why just about every woman is at risk for cervical cancer. The following factors may increase your risk (chance) of cervical cancer:
- Infection with HPV: Most women who develop cervical cancer have had an HPV infection. Among women with persistent HPV infection, not getting screened regularly is the most important risk factor for cervical cancer.
- Sexual activity started at an early age: Cells in the cervix change during puberty and are more vulnerable to damage.
- Sexual activity with many partners: Having many sexual partners can increase your exposure to HPV and increase your risk of getting cervical cancer.
- Sexual activity with a partner who has had many previous sexual partners: If your partner(s) has had many sexual partners, their exposure to HPV is increased and increases your risk of getting cervical cancer.
- Smoking: Smoking can make it less likely that an HPV infection will clear up on its own.
- Pregnancy: Pregnancy causes changes in hormone levels, which may increase your risk of cervical cancer. The more children you give birth to, the greater your risk of cervical cancer.
- Conditions that weaken your immune system: If you’ve been diagnosed with a condition that weakens the immune system, like human immunodeficiency virus (HIV), you may be at a higher risk of getting other infections, like HPV. A weakened immune system can also lower the chances that an HPV infection will clear up on its own. Cells can change more quickly if you’re HIV positive, which can increase your risk of cervical cancer.
If you are concerned about your risk of cervical cancer, talk to your healthcare provider about your plan for screening.
Reduce your risk of HPV (things you can change)
Some of the lifestyle choices you make can lower your risk (chance) of getting HPV, which can reduce your risk for cervical cancer. That’s because this type of cancer is almost always caused by HPV.
- HPV vaccine: Talk to your healthcare provider about the HPV vaccine and whether it’s right for you.
- Limiting sexual partners: Each new sexual partner increases your chance of coming into contact with someone who has an HPV infection. Consider limiting sexual partners. Knowing your partner’s sexual history is also important.
- Safe sex: Practice safe sex by choosing to use condoms — they lower your chance of getting HPV. Keep in mind that the virus may still pass when skin touches skin not covered by the condom.
- Smoking: Don’t smoke and avoid second-hand smoke. Exposure to tobacco smoke can increase the risk of cervical cancer in women with HPV. If you’re currently a smoker, talk to your healthcare provider about options for quitting or cutting back.
HPV is so common that it may be hard to avoid it completely in your lifetime. That’s why it’s important to consider the following to reduce your risk of cervical cancer:
- If you’ve ever been sexually active, have Pap tests regularly starting at age 25, or 3 years after becoming sexually active, whichever is later.
- Have Pap tests regularly even if you’ve had the HPV vaccine. The vaccine doesn’t protect against all types of HPV that can cause cervical cancer.
Visit Healthier Together to learn more about ways to reduce your risk of cervical cancer.
What is the HPV vaccine?
One of the things you can do to protect yourself against HPV is to get the HPV vaccine before you become sexually active (sexual activity includes any skin-to-skin contact in the genital area). If you’re already sexually active, you may still benefit from getting the vaccine. This is because it may protect you from types of HPV you haven’t been exposed to yet. The vaccine can prevent 7 types of HPV that cause about 90% of all cases of cervical cancer.
HPV immunization is currently offered free of charge in Alberta to all girls and boys in Grade 6. Those who don’t receive the vaccine in Grade 6 will be offered the vaccine in Grade 9 and continue to be eligible to receive the vaccine, free of charge, until the end of Grade 12. The vaccine is also available to others for a fee (varies by location). Contact Health Link at 8-1-1 for more information about eligibility and cost.
Here is a short video to learn more about the HPV vaccine: All About HPV, Canadian Cancer Society
To help you decide whether the HPV vaccine is right for you or your child:
- Talk to your healthcare provider
- Visit Immunize Alberta for information about the HPV vaccine
- Use Alberta Health Services’ HPV Vaccine Decision Tool

Remember that even if you decide to get the HPV vaccine, you still need to have a Pap test regularly. The vaccine doesn’t protect against all the types of HPV that can cause cervical cancer, so it’s important to continue getting tested.
Signs and symptoms
It can take a long time for cervical cancer to show any signs or symptoms. This is why screening regularly is so important. Screening can catch cell changes or cancers early, even when you feel completely healthy.
See your healthcare provider right away if you notice:
- Bleeding between periods, after sexual intercourse or after menopause
Other signs and symptoms to look out for include:
- Abnormal, increased, or foul-smelling discharge
- Pain during sex
- Bleeding after a pelvic exam
Remember that experiencing these signs or symptoms doesn’t mean you have cervical cancer, but speaking to your healthcare provider can help you know for sure.