Get Screened
Having regular colorectal cancer screening can prevent and detect cancer at its early stages when treatment is more effective.
Why get screened?
Colorectal cancer is one of the most common cancers in Alberta and affects about 1 in 14 men and 1 in 17 women in their lifetime. Although colorectal cancer can happen at any age, your risk of getting it increases as you get older. Learn more about risk factors that may increase your risk. If you’re between the ages of 50 and 74, it’s important to get screened regularly.1
What is colorectal cancer screening?
Colorectal cancer screening (or colon cancer screening) means looking for early signs of cancer in people who feel well and have no symptoms. Colorectal cancer is easier to treat when found at an early stage. In fact, 90% of cases can be treated successfully if they’re found early.
Although colorectal cancer can happen at any age, your risk of getting colorectal cancer increases as you age. About 90% of cases are in people 50 years of age or older. In Alberta, it is recommended that individuals aged 50 to 74 years get screened with the FIT home stool test every year. After age 74 the benefits of screening may no longer outweigh the risks. Speak with your healthcare provider about your risk for colorectal cancer and when screening may no longer be of benefit.’
Next to age, family history is the most common risk factor for colorectal cancer. If you have a family history of colorectal cancer or polyps, it’s a good idea to talk to your healthcare provider about when you should be screened. Certain risk factors such as family history may mean you start screening at age 40 or even younger.
The 2 main screening tests for colorectal cancer are:
- FIT home stool test This test looks for blood in your stool (poop) that you can’t see. It’s an easy test that you can do at home. If blood is found in your stool, you will need a colonoscopy to make sure the blood isn’t caused by cancer.
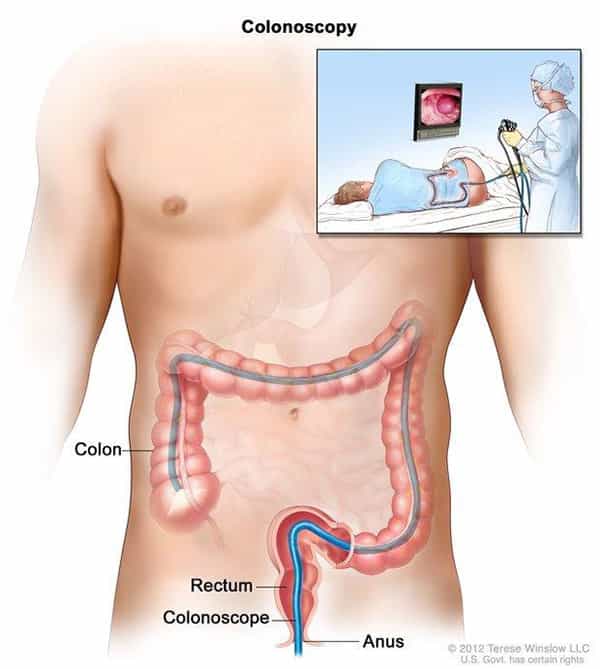
- Colonoscopy: This test lets a healthcare provider see the inside lining of your rectum and colon. This is done with a long, flexible tube called a colonoscope. If polyps or tissue growths are found they can be removed during the test.
Both of these tests find problems early and help save lives. Talk to your healthcare provider about which screening test is right for you and how often you need to have it. Learn more about which test may be right for you.
1. Toward Optimized Practice. Colorectal Cancer Screening Clinical Practice Guideline. November 2013. 2. 2019 Report on Cancer Statistics in Alberta. Surveillance & Reporting. Cancer Research & Analytics, Alberta Health Services.
Who should get screened?
If you’re 50 to 74 years of age, you should be screened regularly. Think of it as part of your regular health routine. If you have a family history of colorectal cancer you may need to start screening at age 40 or younger.
Find out which test may be right for you:
| If… | Then… |
| You’re 50 to 74 years old and have no personal or family history of polyps or colorectal cancer … | Screen with the FIT home stool test every year. |
| You have a first degree relative (parent, sibling or child) that’s had colorectal cancer and/or high risk adenomas, especially if they were younger than 60 when they got it…
Or… You’ve had colorectal cancer before or have been told you have polyps in your colon… |
Colonoscopy is the recommended screening test.
Ask your healthcare provider when you should be screened. Risk factors such as personal or family history may mean you should start screening at age 40 or even younger. |
If you have symptoms of colorectal cancer, whatever your age, talk to your healthcare provider right away.
Symptoms may include:
- Rectal bleeding
- A change in your bowel habits
- Pain in your abdomen
- Losing weight and you don’t know why
Your symptoms may be caused by something other than cancer but to know for sure you can speak to your healthcare provider. Learn more about signs and symptoms at MyHealth.Alberta.ca.
What is a FIT home stool test?
The Fecal Immunochemical Test (FIT) is used to screen for colorectal cancer in people aged 50 to 74 who have an average (or normal) risk for getting the disease. People with an average risk have no personal or family history of the disease. Anyone aged 50 to 74 who is at average risk should screen with FIT every year. Talk to your healthcare provider about your personal risk factors and if FIT is the right test for you.
How FIT works
The FIT checks your stool (poop) for traces of blood that you can’t see. It’s safe, easy to do and can be done in the privacy of your own home.  Common Questions About FIT [info sheet]
Common Questions About FIT [info sheet]
To do the FIT you’ll need to collect a small sample of stool from 1 bowel movement. Easy to follow instructions come with the FIT kit. FIT Lab Instructions [info sheet]
Is FIT right for you?
Talk to your healthcare provider about colorectal cancer screening and ask if the FIT is the right screening test for you.
What to expect with FIT
The FIT checks your stool (poop) for traces of blood that you can’t see. It’s safe, easy to do and can be done in the privacy of your own home.
- How do I get a FIT kit?
There are two easy ways to get a free FIT kit:
1. Talk to your healthcare provider. They’ll give you a lab requisition form. Take this form to the lab to pick up your FIT.
2. Order online at screeningforlife.ca or call AHS Screening Programs toll-free at 1-866-727-3926. We’ll mail you a FIT.
If you need a healthcare provider:
• Visit albertafindadoctor.ca
• Call Health Link at 8-1-1
• Visit search.cpsa.ca
(College of Physicians & Surgeons of Alberta)
- How do I do the FIT test?
The FIT kit comes with easy to follow instructions. You’ll need to collect a small sample of stool (poop) from 1 bowel movement. After collecting your stool sample, you’ll take your completed FIT kit back to the lab. The lab will then test the sample for any hidden blood.
FIT Lab Instructions [info sheet]
- Getting your FIT results
Your FIT result will be sent to your healthcare provider who will follow-up with you directly. Learn more about getting your FIT results.
Benefits and risks of FIT
As with any test, there are both benefits and risks.
Benefits of doing a FIT
A FIT is easy to do, safe and won’t hurt. It can detect traces of blood in your stool that you can’t see. If any blood is found, the recommended follow-up test is a colonoscopy. A colonoscopy may find any precancerous polyps or cancer at its early stages, when treatment can work better.
Risks of doing a FIT
The FIT does run the risk of missing blood in the stool, because a polyp or cancer may not bleed at the time you take the test. This is why screening with FIT every year gives you the best chance of colorectal cancer being found early, when treatment can work better.
Frequently asked questions about ordering a FIT kit
I don’t have a family doctor. Can I still order a FIT?
Yes, you can still order a FIT online or by phone. However, if your FIT result is abnormal, it’s important that you make an appointment with a doctor or healthcare provider to discuss follow-up testing. If you need help finding a family doctor visit ahs.ca and click on ‘Find Healthcare’ or call Health Link at 8-1-1.
My family doctor has given me a requisition form to take to the lab and pick up my FIT kit. Can I order it online instead and have it mailed to me?
No, if you already have a lab requisition for a FIT please take this form to your nearest lab and pick up your FIT kit instead of ordering one online or by phone.
How will my FIT kit be shipped?
Your FIT should arrive by Canada Post, in a discrete envelope, within 10 business days. If it’s been over 3 weeks and your FIT kit has still not arrived, please call AHS Screening Programs toll-free at 1-866-727-3926, Monday to Friday, 8:00am to 4:30pm.
My FIT kit was lost or damaged. Can I order a new one?
Call AHS Screening Programs toll-free at 1-866-727-3926, Monday to Friday, 8:00am to 4:30pm to order a new FIT kit.
I am having a problem with my FIT order. What should I do?
For assistance, please call AHS Screening Programs toll-free at 1-866-727-3926, Monday to Friday, 8:00am to 4:30pm.
Why is Dr. Huiming Yang’s name listed on my FIT lab requisition?
Dr. Huiming Yang is the Medical Director of AHS Screening Programs. In his role as Medical Director, he initiated the FIT ordering process so that you could have the test mailed directly to you. Dr. Yang is the ‘ordering’ or ‘authorizing’ provider on your FIT lab requisition form. Dr. Yang is not meant to replace your regular health care provider.
Completing your FIT:
I made a mistake collecting my stool sample. What should I do?
Call AHS Screening Programs toll-free at 1-866-727-3926, Monday to Friday, 8:00am to 4:30pm to order a new FIT kit.
I got my FIT kit in the mail a while ago but haven’t done it yet. Does the test expire?
Yes, FITs do expire. Please check the expiry date on your FIT collection container. If your FIT has expired, please discard. Call AHS Screening Programs toll-free at 1-866-727-3926, Monday to Friday, 8:00am to 4:30pm, to order a new FIT kit.
How soon after collecting my sample do I take it to the lab?
You need to take your FIT and lab requisition form to the lab within 7 days of collecting your sample.
Do I need to make a lab appointment to drop off my completed FIT?
No, you do not need an appointment to drop off your FIT kit.
Where is my nearest lab for FIT drop off?
For lab locations and hours of operations visit:
- Albertaprecisionlabs.ca or call 1-877-868-6848
How do I get my results if I ordered my FIT online or by phone?
You can view your FIT results online if you have a MyChart (formerly MyAHS Connect) account. MyChart is available to all MyHealth Records users.
If you have an abnormal result, you’ll also receive a letter by mail from the Alberta Colorectal Cancer Screening Program. Normal result letters will not be mailed to Albertans who have a MyChart account.
Will my FIT result be sent to my family doctor if I ordered my FIT kit online or by phone?
If your result is abnormal you will need to make an appointment with your family doctor or regular healthcare provider to discuss the need for a colonoscopy. If you do not have a regular healthcare provider your result letter will provide a list of resources to help find a family doctor in your area.
You will need to book an appointment with your family doctor as soon as possible to discuss your abnormal result and follow-up testing.
What is a colonoscopy?
A colonoscopy test lets your doctor see the inside lining of the colon and rectum. This is done with a colonoscope, which is a long, thin, flexible tube with a light and small video camera on the end. This test will help your doctor know if there are polyps or cancer in the colon and or rectum.
To get a colonoscopy in Alberta you need a referral from your doctor or walk-in clinic. If a colonoscopy is the right test for you, your doctor will recommend you have one and arrange your referral. A colonoscopy is not a test you can request or arrange on your own.
Why a colonoscopy is done
Your doctor may recommend a colonoscopy to:
· Follow up after an abnormal FIT result (Fecal Immunochemical Test). An abnormal FIT (poop test) means blood was found in the stool. When blood is found in the stool, important to find out what may have caused it. Most often, a colonoscopy test is recommended.
· Check on symptoms. A colonoscopy can help your doctor investigate and find the cause of symptoms such as rectal bleeding, abdominal (belly) pain, a change in bowel habits, and unexplained weight loss.
· Monitor after colorectal treatments.
· Screen for colorectal cancer. If you have a personal or family history of colorectal cancer or high-risk polyps (a type of polyp that can turn into cancer if it is not removed) your doctor may recommend a screening colonoscopy test.
Watch these 2 short videos to learn more about colonoscopy.
Video 1: What is a colonoscopy and why do I need one? (05:38)
Learn about the colonoscopy test, and its benefits, and risks.
Printable handout:
My doctor wants me to have a colonoscopy
Video 2: What to expect during and after your colonoscopy (07:41)
This video will guide you through the entire process of a colonoscopy test.
The risks and benefits of getting a colonoscopy
Overall, a colonoscopy is safe. But, like any medical test, there’s a small chance that problems can occur.
· Before having a colonoscopy, you’ll need to drink a strong laxative medicine to clean out your colon. This can sometimes cause nausea, vomiting, dehydration, or dizziness. Severe dehydration can cause falls, electrolyte imbalances, or kidney issues. Electrolytes are minerals that your body needs. The best way to prevent dehydration is to drink lots of clear fluids.
· For the test, most people have sedation medicine through an intravenous line or IV to help them feel calm and comfortable. Rarely, problems from sedation medicine can occur, including, low blood pressure, breathing problems, or an allergic reaction.
· Although the test is very thorough, there’s a chance that cancer or polyps could be missed.
· Bleeding can happen where a polyp is removed, or a tissue sample is taken.
· Rarely, a colonoscopy can cause a hole or tear in the colon.
· Infection can occur in the colon, or at the IV site.
· If a serious problem happens, you might need surgery, antibiotics, or a blood transfusion. In extremely rare cases, damage to nearby organs or a serious complication from a colonoscopy can result in death.
The benefits of a colonoscopy
Although the risk of a serious problem is very low, there are many benefits of having a colonoscopy.
It can help diagnose problems in the bowel and can also prevent colorectal cancer by finding and removing polyps. When colorectal cancer is found early, 90% of cases can be treated successfully.
The number of people who benefit from a colonoscopy is much higher than the number who have problems. Talk to your healthcare provider if you have any questions or want to discuss alternatives to a colonoscopy.
More information
To find out more about colonoscopy, go to ahs.ca/colonoscopy or speak with your healthcare provider.
Where to get screened
In Alberta, getting screened can be done easily right at home. If you’re 50 to 74 years old there are two easy ways to get a free FIT test. Choose what works best for you.
- Talk to your healthcare provider about colorectal cancer screening. If FIT is the right test for you, they’ll give you a lab requisition form. Take this form to the lab to pick up your FIT.
OR
- Order online at screeningforlife.ca or call AHS Screening Programs toll free at 1-866-727-3926. We’ll mail you a FIT.
If you or a first degree relative (parent, sibling, child) have had colorectal cancer and/or high risk adenomas, especially if they were younger than 60, ask your healthcare provider if a colonoscopy is the right test for you. Certain risk factors such as personal or family history may mean you should start screening at age 40 or younger.Here are some questions you may want to ask your healthcare provider about colorectal cancer screening:
- Do I need to get screened for colorectal cancer?
- What are my risk factors for colorectal cancer?
- Is the FIT home stool test right for me?
- What are my screening options? How are they different?
- What are the benefits and risks of colorectal cancer screening?
If you don’t have a healthcare provider, check out these resources to help find one:
- Visit Alberta Find a Doctor
- Call Health Link at 8-1-1
- Visit Inform Alberta
- Visit the College of Physicians and Surgeons of Alberta
Remember, getting screened is the single most important thing you can do to protect yourself against colorectal cancer.
Other colorectal cancer screening tests
While the FIT home stool test and colonoscopy are the 2 most common screening tests, there are also other colorectal cancer screening methods. Any abnormal results should still be followed by a colonoscopy for the tests described below. Talk with your healthcare provider about which screening test is right for you.
- CT colonography: This is a CT scan taken of the colon after bowel cleansing to get an accurate picture of the lining of the rectum and colon. This test is usually done at private radiology clinics and is not covered by the Alberta Health Care Insurance Plan. If a polyp is found, it’s recommended that you have a colonoscopy to remove the polyp, as the CT only looks at your colon.
- Flexible sigmoidoscopy: This test uses a colonoscope to examine only the lower left side of the large bowel. If a polyp is found, it’s recommended that you have a colonoscopy to examine the other side of the colon. A flexible sigmoidoscopy is usually done every 5 years.
Research into new colorectal cancer screening tests.
- Shield™: A new blood test for colorectal cancer screening. Shield™ detects DNA molecules shed by cancer and pre-cancer cells into the bloodstream. If cancer cells are detected the patient will need to have a follow-up colonoscopy. Shield was recently approved by the FDA for use in the Unites States. It is currently not a recommended colorectal cancer screening test in Alberta or anywhere in Canada at this time. The Alberta Colorectal Cancer Screening Program will continue to review the evidence for the use of this test as it becomes available.
- PolypDX™: Alberta is starting to test a new approach to colorectal cancer screening using a urine test called PolypDX™. This test detects pre-cancerous polyps in the colon. If polyps are found, the follow-up test is a colonoscopy. PolypDX™ isn’t available to Albertans.
Colorectal Cancer Screening for the 2SLGBTQI+ Community
We’re keeping up with the latest research about cancer screening for 2SLGBTQI+people. We’ll be regularly updating this section with input from our 2SLGBTQI+ partners and emerging evidence.
Last updated December 2023.
Screening Programs is pleased to share three new information sheets on cancer screening that have been designed for the 2SLGBTQI+ community.
Cancer Screening for the 2SLGBTQI+ Community
Download [info sheet] 
Breast/Chest Cancer Screening for the 2SLGBTQI+ Community
Download [info sheet] 
Cervical Cancer Screening for the 2SLGBTQI+ Community
Download [info sheet] 
Colorectal cancer screening is for everyone
It’s important for everyone of any gender identity or sexual orientation to get screened for colorectal (or colon) cancer between the ages of 50 to 74. Sexual orientation or gender identity doesn’t affect your risk of colorectal cancer and won’t change how you’re screened.
Get screened every year using FIT (the Fecal Immunochemical Test). FIT is an easy at-home screening test that checks for hidden blood in your stool (poop).
Receptive anal sex (bottoming) and colorectal cancer screening
You can keep having anal sex before and after you’ve collected your stool sample for a FIT test and before and after your colonoscopy.
Gender-affirming hormone therapy and colorectal cancer
We don’t know if testosterone, estrogen or progesterone are risk factors for colorectal cancer. There’s no evidence either way. What we do know is that healthcare providers don’t need to know a person’s hormone levels when screening for colorectal cancer. For example, a healthcare provider won’t ask someone if they’re on birth control.
Citations: Canadian Cancer Society
How Can I Get Screened?
There are two easy ways to get a free FIT home stool (poop) test:
1. Talk to your healthcare provider. They’ll give you a lab requisition form. Take this form to the lab to pick up your FIT.
2. Order online at screeningforlife.ca or call AHS Screening Programs toll-free at 1-866-727-3926. We’ll mail you a FIT.
If you need a healthcare provider:
• Visit albertafindadoctor.ca
• Call Health Link at 8-1-1
• Visit search.cpsa.ca
(College of Physicians & Surgeons of Alberta)
Gender affirming clinics and providers:
- DX Medical Centres – Medical Clinic in Edmonton
- Wellness Centre in Edmonton
- Dr. Jillian DeMontigny (Haig West Family Health Care Clinic in Lethbridge)
- Justik Medical Clinic – Family Medicine Clinic in Edmonton
- Dr. Ted Jablonski and others (Pinnacle Medical Centres in Calgary and surrounding area)
- Skipping Stone
- Telus Virtual Health (province-wide)
- The Alex in Calgary
- The Pride Centre in Edmonton
- Trans Wellness Initiative (province-wide)
Gender affirming clinics and providers – Indigenous:
- Elbow River Healing Lodge in Calgary
- Indigenous Wellness Clinic in Edmonton
- Dr James Makokis (South Common Medical Clinic in Edmonton)
*Please note, some clinics may not be accepting patients at this time. Contact the clinic directly to find out if they are accepting patients, have a waiting list, or can provide a referral.
For More Information
Cancer Screening for the 2SLGBTQI+ Community
Download [info sheet] 
Breast/Chest Cancer Screening for the 2SLGBTQI+ Community
Download [info sheet] 
Cervical Cancer Screening for the 2SLGBTQI+ Community
Download [info sheet] 
LGBTQ2S+/Sexual and Gender Diversity, Alberta Health Services
Sexual and Reproductive Health, Alberta Health Services
For 24/7 nurse advice or general health information, call Health Link at 811.
Colorectal Cancer Screening for First Nations People
The following resource about colorectal cancer screening was developed for First Nations people by the Alberta First Nations Information Governance Centre. Alberta FNIGC Colorectal Screening




